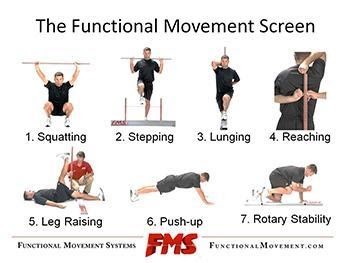
There are seven movement competencies assessed in the FMS; these are:
Overhead Squat
How:
Feet shoulder-width apart
Knee over foot
Dowel over foot
Torso and tibia parallel
No valgus collapse in the knee
NB: Butt-wink is not an issue
Hurdle Stepping
How:
Adopt a single leg stance
Line up the string or top of the hurdle with the tibia tuberosity
Assess if they can maintain stable torso and head
Step over and clear hurdle
In-line Lunge
How:
Adopt a split stance
Keep dowel touching: Head, thoracic spine and sacrum
One joint, e.g. hip, knee, ankle or poor core stability, could affect the whole movement pattern. Correcting the dysfunction will correct the movement pattern.
These first three movements are challenging and can expose limitations and compensatory movement. The hurdle step and in-line lunge mimic the split stance, unilateral nature of life and many athletic tasks.
Shoulder Rotators
How:
Reach one hand/arm over the top of your shoulder
Reach the other hand/arm behind your back
Make a fist with both hands and try to touch each one
If the hands are within: one hand length = 3; 1 and ½ hand lengths = 2; > 1 and ½ hand lengths = 1; pain = 0
The shoulder rotator test is a clearing test that measures shoulder health and mobility as well as thoracic spine mobility, both of which help the overhead squat. If the squat is poor, it could be the result of the shoulder rotators and dysfunction through the thoracic spine.
Hamstring ROM Lift
How:
Position the client in neutral, e.g. no external or internal rotation through the hip
Place the dowel at “mid-thigh,” e.g. halfway between the knee and the ASIS of the non-assessed limb.
If the malleolus of the ankle on the assessed limb, can reach past mid-thigh with no knee bend and hips remain neutral, record a 3
Between the knee and the dowel, record a 2
Can’t go past the knee, record a 1
If pain is evident record a 0
If a client demonstrates incompetency during the hurdle step or in-line lunge, it could be due to poor hamstring ROM. If the client cannot get their leg 6 inches off the ground, then there is the mobility issue.
Push up
How:
Position client in the push-up position. Hands should be just outside shoulder-width apart
Hand placement should result in thumbs being just above the forehead
The client must maintain good posture through the torso and spine
If the client cannot perform one repetition in this position, or if they are female, position hands so that thumbs are in line with the chin
If the client cannot perform one repetition in this position, position their hands so that their thumbs are in line with the shoulder joint
If the client cannot perform one repetition in this position, they achieve a 1.
An assessment of trunk stability.
Rotary Stability
How:
Get the client positioned on all fours.
Get the client to extend the arm and leg on the same side of the body.
From this extended position, get the client to bring their arm and leg back towards the starting position and ask that they attempt to touch the elbow to knee.
If the client can perform this with minimal issue or loss of balance, then they score a three. If they do not score a three then have the client perform the same movement with alternate sides, e.g. left arm and right leg. Doing this would result in a score of 2.
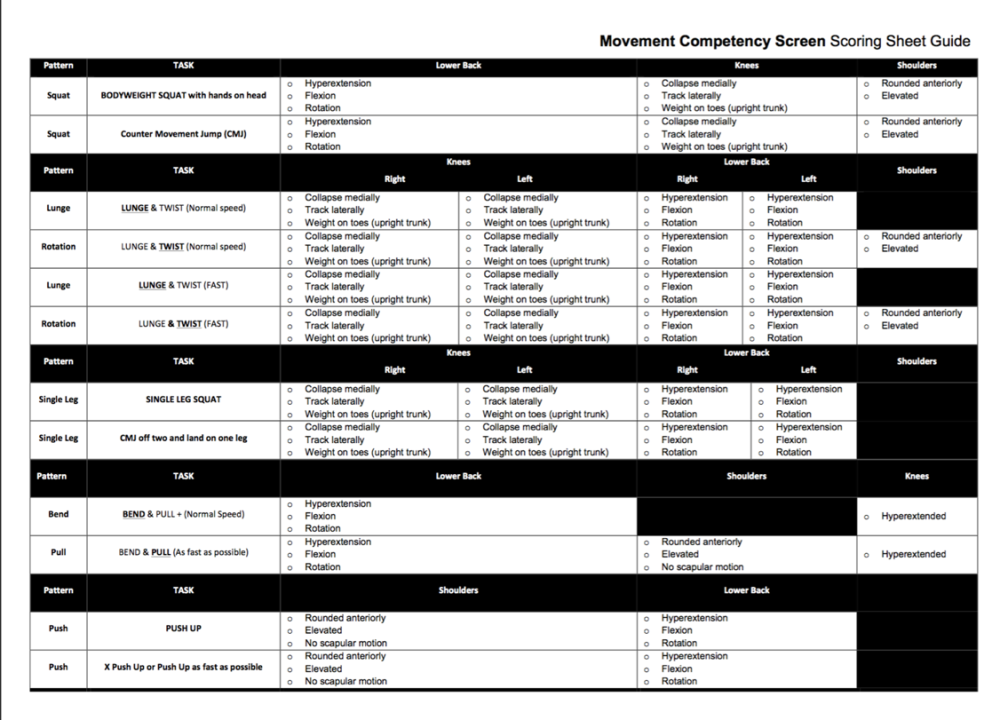
Movement Competency Screen
The MCS also helps determine an individual’s movement competency to help practitioners gain an understanding of how their clients move and whether or not the movement they produce is free of dysfunction and pain. Numerous variables can influence the movement competencies of an individual (Gamble n.d.). However, the premise behind the screen is to develop an understanding of how an individual can move, so their prescribed training does not exceed their capabilities (Gamble n.d.). Therefore, the MCS is a tool used to ascertain if a practitioner can assertively load a particular pattern, or if a developmental approach would be better suited to the individual.
There are 11 movement tasks within the MCS:
1) Bodyweight Squat
2) Countermovement Jump
3) Lunge and Twist (Slow)
4) Lunge and Twist (Fast)
5) Bilateral broad jump with unilateral landing
6) Push up
7) Explosive push up
8) Bend and pull (Slow) NB: Performed like a Pendley row.
9) Bend and pull (Fast)
10) Bodyweight single leg squat
11) Bilateral countermovement jump with single-leg landing
The unilateral tasks are completed on both sides of the body. Instruct the individual to perform 2-4 repetitions of each movement task.
For a video on how to complete these movements, please refer to the following link.
https://www.youtube.com/watch?v=EMU0bM7ACAM